What Are Some Innovative Technologies Used In Neurorehabilitation?
Imagine harnessing the power of cutting-edge technology to heal your brain and improve your quality of life. This isn’t the plot of a sci-fi movie— it is the day-to-day reality for many patients undergoing neurorehabilitation. Emerging technology in this field boasts the potential to revolutionize treatment for brain injuries and disorders. In this article, you’ll discover some of these transformative techs and how they are paving the way for the future of neurorehabilitation.

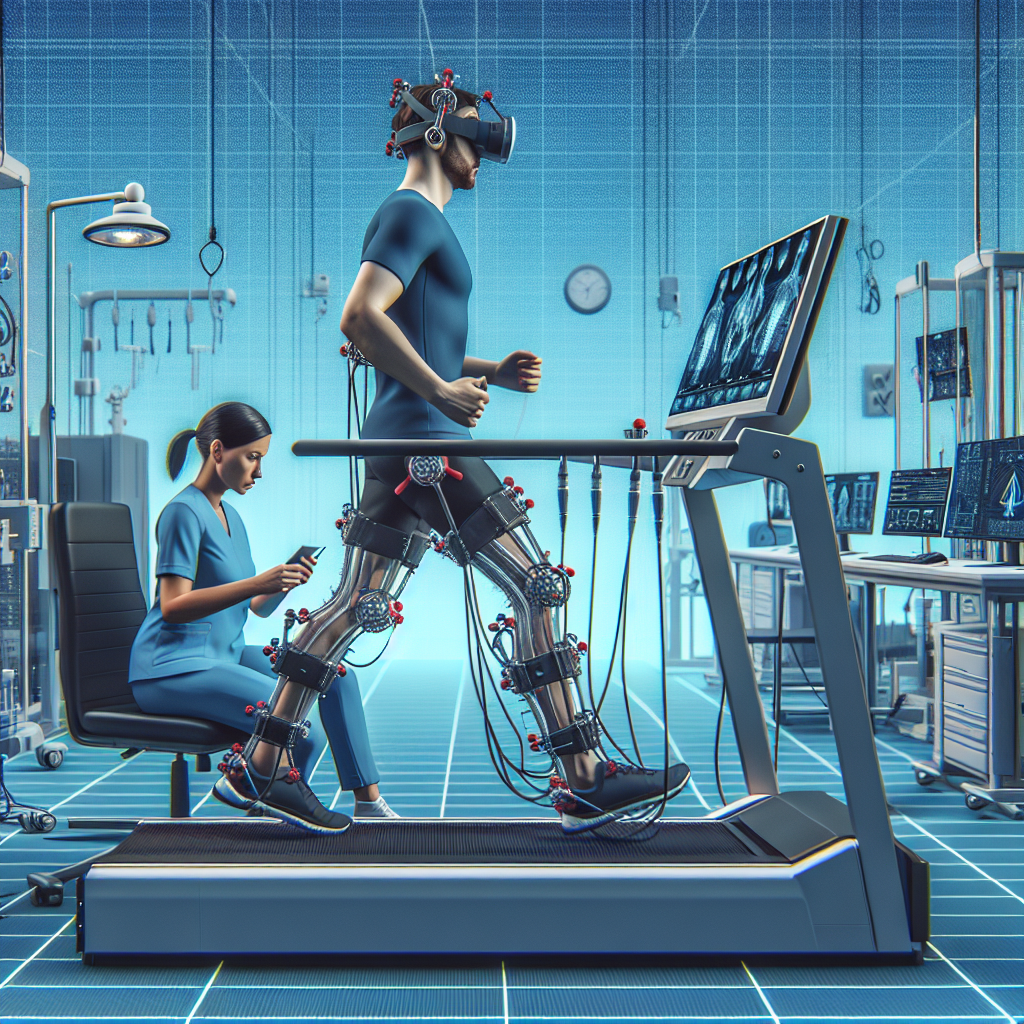
Virtual Reality in Neurorehabilitation
Imagine this: You’re wearing a headset, completely immersed in a simulated world. You’re not just playing a video game, you’re involved in groundbreaking Virtual Reality (VR) therapy.
Understanding the basics of Virtual Reality
Virtual Reality utilizes computer technology to create a simulated, three-dimensional world that a user can manipulate and explore while feeling as if they are in that world. VR systems typically include a headset fitted with sensors, which track the direction in which you’re looking, adjusting the view accordingly.
Applications in Stroke Neurorehabilitation
For stroke survivors, VR technology offers a unique opportunity to enhance their motor and cognitive skills while remaining in a controlled environment. In terms of neurorehabilitation, VR provides precise, repeatable, and intensive training scenarios, which have been shown to benefit neuromuscular control and enhance recovery.
Benefits and limitations of VR technology
VR technology has the potential to transform neurorehabilitation. It captures a wealth of data, enabling professionals to assess and adjust treatment plans. VR also motivates and engages patients to a significant extent. On the other hand, VR technology’s limitations include its expensive cost and the need for patients to adapt to the virtual environment, which can be difficult for some.
Robot-Assisted Therapy
In this age of smart technology, robots step in to assist with various aspects of neurorehabilitation, making it more precise, customized, and effective.
Principles of Robot-Assisted Therapy
In Robot-Assisted Therapy (RAT), robots play a significant role in assisting patients regain physical skills. Via RAT, patients get to practice specific tasks repeatedly with the assistance and support of the robot. It operates on the principle of neuroplasticity–the brain’s ability to reorganize itself by forming new neural connections.
Role in Spinal Cord Injury Rehabilitation
For spinal cord injury patients, RAT enhances the strength, coordination, and overall mobility skills. Robots help in improving walking ability by providing body-weight support and mimicking the regular walking pattern, enabling patients to relearn certain movements.
Robot-Assisted Therapy for stroke survivors
RAT significantly aids stroke survivors. For instance, robotic arms support paralysed or weakened limbs, enabling stroke survivors to engage in repetitive motor activities which further assist in reactivating neural pathways for better post-stroke outcomes.
Functional Electrical Stimulation (FES)
FES is an effective neurorehabilitation method that can encourage muscle contraction and use after paralysis.
Mechanism of FES
The principle behind FES lies in the application of brief electrical pulses to paralyzed muscles, causing them to contract and perform functions akin to their natural role. For instance, when applied to leg muscles, it can enable walking.
Use of FES in Motor Recovery
In the context of motor recovery following a stroke or spinal cord injury, FES helps in improving muscle strength, reducing muscle shrinkage, and improving blood circulation.
Advantages and Challenges of FES
While being a promising tool for neurorehabilitation, FES also poses certain challenges. The process may not be suitable or have less efficacy for patients with certain conditions. It can also cause discomfort and requires health professionals to have specific technical expertise.
Transcranial Magnetic Stimulation
Transcranial Magnetic Stimulation (TMS) is a non-invasive procedure used to stimulate small regions of the brain for therapeutic purposes.
Understanding Transcranial Magnetic Stimulation
During the TMS procedure, a magnetic field generator produces small electrical currents in the region of the brain just under the coil via electromagnetic induction.
TMS and Stroke Rehabilitation
The potential role of TMS in stroke rehabilitation lies in its ability to modulate neuroplasticity, eventually leading to functional recovery. By targeting specific brain areas, it helps improve motor skills and alleviate post-stroke depression symptoms.
Benefits and obstacles of TMS
TMS provides a valuable tool for personalizing post-stroke therapy, improving the efficiency of physical and cognitive rehabilitation interventions. However, few limitations surround the method: specificity and intensity of stimulation, patient’s age, and time elapsed since stroke.
Neurofeedback Therapy
Neurofeedback therapy represents a crucial component in the progressive world of neurorehabilitation.
Understanding Neurofeedback Therapy
In neurofeedback therapy, electronic sensors are used to monitor brain waves using EEG (Electroencephalography). The feedback helps train the brain to operate more efficiently.
Neurofeedback approaches in treating brain injuries
Our brain’s natural ability to self-regulate is inevitably disturbed after brain injuries. Neurofeedback can help reinstate this capacity, making it a potentially effective treatment.
Impacts and restrictions of Neurofeedback Therapy
Neurofeedback demonstrates potential in addressing a variety of neurological conditions. However, the technique demands specialized professional expertise and can be time-consuming.
Brain-Computer Interface (BCI)
The decentralized and interactive nature of BCI marks a revolutionary step in neurorehabilitation.
Understanding Brain-Computer Interface
A BCI directly measures the user’s brain signals and translates them into commands, reaching an external device. Such a system doesn’t rely on the brain’s normal output pathways of peripheral nerves and muscles, providing new communication and control avenues.
Role of BCI in Neurorehabilitation
In the field of neurorehabilitation, BCIs are being used to restore mobility, communication, and independence to individuals suffering from paralysis or severe motor impairments.
Future potential and limitations of BCI
The potential of BCI in neurorehabilitation is vast. However, limitations include the need for extensive training, technological challenges related to durability and reliability of the system, and ethical considerations.
Neuroprosthetics and Assistive Devices
Welcome to the era of Neuroprosthetics, where technological advancements are revolutionizing neurorehabilitation processes.
Introduction to Neuroprosthetics
Neuroprosthetics are artificial devices or systems designed to substitute or improve functions of impaired nervous systems. This innovative therapy aims to restore functions such as hearing, sight, movement, and even cognitive processes.
Impact on improving life quality
By replacing or enhancing functions, neuroprosthetics markedly improve the individuals’ ability to perform daily activities, thereby enhancing their overall quality of life.
Challenges and future of Neuroprosthetics
While showing promising advancements, the field faces challenges like device integration, user acceptance, and regulatory hurdles. However, ongoing research and developments in this field suggest a bright future.
Telerehabilitation
Physical distancing needn’t mean cutting off therapeutic support. Say hello to Telerehabilitation!
Understanding Telerehabilitation
Telerehabilitation is the provision of rehabilitation services over telecommunication networks and the internet. The substantial growth in internet-based communication tools has made telerehabilitation possible.
Telerehabilitation in managing neurological disorders
Telerehabilitation has shown feasibility and effectiveness in managing a range of neurological disorders, including stroke and Multiple Sclerosis. By providing home-based, customized rehabilitation programs, it ensures continuity of care and maximizes functional recovery.
Advancements and barriers in Telerehabilitation
While Telehabilitation brings various advantages like accessibility, cost-effectiveness, and customization, challenges persist. These include ensuring privacy and safety, managing technical difficulties, and navigating variable regulatory landscapes.
Neurogaming and Gamification
Experience therapy as a fun-filled journey. Yes, it’s possible through neurogaming and gamification!
Understanding Neurogaming and Gamification
Neurogaming combines neuroscience with video game design, creating immersive, adaptive experiences aimed to improve cognitive capabilities. Gamification, on the other hand, includes applying game-design elements and game principles in non-game contexts.
Role in improving cognitive and motor skills
Game-based neurorehabilitation can enhance patients’ motivation, thereby improving adherence to treatment plans. Both neurogaming and gamification have shown promise in improving cognitive and motor skills among neurologic patients.
Possibilities and limitations of Neurogaming
The possibilities opened up by neurogaming and gamification are vast. Yet, limitations such as the need for technical skills, potential risk of addiction, and ensuring the quality of game design are potential challenges that need to be considered.
Deep Brain Stimulation
With Deep Brain Stimulation (DBS), you’ll witness how neurorehabilitation is undertaken at a deeper level.
Basics of Deep Brain Stimulation
Deep Brain Stimulation involves implanting electrodes within certain regions of your brain. The implanted electrodes produce electrical signals that modify abnormal signals of the brain, offering symptomatic relief to patients.
DBS in Parkinson’s disease treatment
DBS is applied in treating conditions like Parkinson’s disease, where it assists in managing symptoms such as tremor, rigidity, and problems with walking and speech.
Advantages and detriments of DBS
DBS offers a powerful tool to manage neurodegenerative disorders. However, it doesn’t stop disease progression, and potential side effects include surgical complications, speech issues, and cognitive decline.

